Pigmentation and its many masters
Dermal Aesthetics
What is pigmentation?
The colour of your skin, hair and eyes are influenced by the level of melanin (pigment) in your genetic makeup, as well as the level of exposure (inflammatory response) to sun. For most of us, our pigmentation (skin colour) will deepen when we are in the sun, resulting in a tan. However, when we refer to ‘treating pigmentation’ in the beauty industry, we are referring to the uneven blotches of melanin that has resulted in sun spots, freckles, melasma etc. Pigmentation caused by UV, in most cases, is easy to treat with laser and peels etc. Where pigmentation has been caused by factors other than UV, it becomes trickier to treat.
Melanin has the ability to absorb UV rays and the melanocyte cell will deposit it over our cells like an umbrella to protect our precious DNA. The melanocyte cell is called to action when it is stimulated. This stimulation can be triggered by a number of sources as this cell answers to many masters.
Pheomelanin and eumelanin are the two forms of melanin that are present in all skins, but in differing amounts. More pheomelanin produces red to yellow pigment (fairer skins) whereas eumelanin produces brown to black (darker skins). Pheomelanin is less stable and can generate mutagenic cells, therefore lighter skins are more at risk of UV damage. Eumelanin actually has radio and photoprotective properties.
Normal skin will contain 1000 melanocytes per sq mm. These melanocytes can produce 100 melansomes per day which forms the melanin (you can think of it as melanosome poo). One melanocyte pigments up to 36 Keratinocytes cells (which are the predominant cells found in the epidermis) by injecting its melanin with needle like dendrites. It is then carried up to surface. The pigment becomes bleached at the Stratum Lucidum and then disintegrates. Even black skinned people shed white dead cells. Interesting fact: The amount of melanocyte cells is exactly the same in all skin colours but the amount of melansomes and type of melanin will differ genetically. White skinned people have melanin in the sub epidermis but black skinned have melanin everywhere even in the pores.
Types of pigmentation:
- Melasma: addressed further down, as this condition requires a completely separate discussion from regular (UV) pigmentation.
- Chloasma: Is specific to pregnancy and is a temporary form of melasma. It can cover the face and even the stomach and will worsen in UV. It is often called the mask of pregnancy and is identical on both sides (like butterfly wings). It will generally fade when the hormones are balanced again.
- Solar Lentigines: Also called age, sun or liver spots these are benign flat brown spots that look like large brown freckles. 90% of fair skinned people (type 1 and 2) over the age of 60 develop these.
- Poikiloderma is a skin condition that consists of areas of hypopigmentation, hyperpigmentation, telangiectasias and atrophy (thinning of the skin). Cause in unknown but some likely links found can be: hereditary, Lyme disease, lupus, steroids, radiation treatment, UV exposure, change in hormones (especially lower eostrogen), chemical reaction to perfume, Poikiloderma of cuvette is most frequently seen on the check or the neck and characterised by red colour pigment that is commonly associated with sun damage. Treatments used are bleaching creams such as hydroquinone, needling and IPL.
- Ephelides (freckles): Freckles are common and generally hereditary.
- Vitiligo: This is a form of hypo pigmentation caused by the LOSS of pigment producing cells for which there is no known cure. It presents as white patches that are extremely sensitive in sun and is most common in those with darker skins. It is considered an autoimmune disorder. Full repigmentation is rare. Hydroquinone can be used to fade the darker area of skin to even out the skin tones.
- Post inflammatory Hyper Pigmentation: Occurs after an injury to the skin. Most common in acne sufferers
Pigmentation triggers may include:
- UV exposure
- Hormonal fluctuations such as pregnancy and menopause. During pregnancy estrogen is higher and an excess can stimulate melanocyte cells
- Medications such as the pill, anti depressants, antiseptics, heart medications, anti anxiety, anti inflammatory’s, acne medications, antibiotics, anti-fungals and some blood pressure medications and steroids
- Free radicals because they stimulate the release of chemicals that induce the melanocyte to make more melanin
- Alcohol, synthetic fragrance and cigarettes
- Acne scarring and trauma to the skin
- Vitamin A, C and D deficiency
- Stress can trigger the hormone cortisol which also causes inflammation
- Underactive thyroid (hashimoto)
- Artificial light from computer screens and fluoro lighting can stimulate pigment through the retina of the eye.
Pigmentation pathways
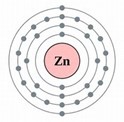
Pigmentation is regulated by over 125 genes. Overproduction of melanin mostly occurs in the epidermis and has following process. Understanding the steps in the process (called melanogenesis) also gives us opportunity to intervene in these steps:
- A trigger occurs (as per above triggers) that will stimulate a hormone called, Melanin stimulating hormone (MSH). This signals BOTH the melanocyte and keratinocyte cells.
- Next a copper converting enzyme called Tyrosinase is activated and this contributes to tyrosine oxidation. This enzyme is the same one found in the plant world that turns a banana or a mushroom brown.
- Tyrosinase converts the amino acid called Tyrosine to DOPA which assists in melanin formation in the melanosome
- The chemical pathway then splits and the Dopa Quinone and Dopa Phosphates are created. They are pheomelanin and eumelanin pigment building blocks within melanosome that produce the melanin within melanosome
- Transfer of the pigment is then injected into Keratinocyte and the melanosomes then arrange themselves on the side of the assault like a protective umbrella to protect the cells nucleus
Current Proven Ingredients
- MHS inhibitor –sunscreen. Melanin is actually our body’s natural sunscreen. If we use sunscreen our body (MSH) will not need to manufacture it. But not just any sunscreen – blue light filters are paramount. (stage 1)
- Tyrosinase inhibitors– L-Ascorbic Acid, Arbutin (AKA bearberry), Tretinoin, Hydroquinone, Liquorice, St Johns Wort, Yarrow, Arnica, Daisy flower, Kojic Acid (derived from fungus), Mallow, Thyme, Azelaic Acid, Gluconic Acid, Paper Mulberry (only 0.396% was required to inhibit the tyrosinase in comparison to 5.5% hydroquinone and 10% kojic acid)– (stage 3)
- Melansome Transfer inhibitors – Arbutin, retinoids and Niacinamide (B3) all halt the transfer of melanin – (stage 5)
Exciting NEW ingredients
Plasminogen inhibitor- There is a vascular component in Melasma. A newly emerging ingredient that has a mounting evidence in reducing vascularization is Tranexamic Acid. It is a synthetic lysine amino acid derivative which blocks the conversion of plasminogen to plasmin. Plasmin is involved in inflammation. By blocking the plasmin there is less free arachidonic acid production, prostaglandin levels and fibroblast growth factor, (ALL players in our inflammation pathway), which in turn reduces tyrosinase activity. In addition, it blocks the transfer of pigment from melanocytes to keratinocytes in the epidermis. All of this helps in reducing hyperpigmentation. It is recommended to use after Vit C in morning and retinol in evening. Gluthathione will also strengthen immune system, improve mental function, sleep, prevent Alzheimers and support liver and support chemo patients.
Glutathione is one of the most powerful antioxidants produced in the liver. It can inhibit Tyrosinase and there has been a huge surge of treatments administering intravenous GSH for general skin lightening. It can prevent damage to cellular components caused by ROS, such as free radicals and peroxides etc. Oral bioavailability is considered low and one report I read confirmed whilst it can easily reach blood stream, there is no guarantee it can penetrate the cells. Another report recommended to increase ingredients that can assist the body in manufacturing naturally. Perhaps because we know if the body does not make something itself it will fight to break it down. Raw materials of cysteine and glycine can help manufacturer it. Calcitriol (d3) increases it. Of further interest to me was that melasma is considered a by product of a dysfunction in the liver and Gluthathione is produced in the liver. I was unable to find conclusive evidence that Glutathione does impact melasma, (unlike TA) but I think more research is not far away.
Not New: but a word about Hydroquinone
Hydroquinone – has been the gold standard for skin whitening for many years but it comes with side effects. It cannot be used long term as it can result in rebound pigmentation, irritation, redness, dermatitis, thin skin, dilated capillaries and fungal acne. There is also a rare risk of developing ochronosis (bluish/black pigmentation), which is a paradoxical reaction to the hydroquinone resulting in permanent discolouration due to permanent loss of melanocytes due to oxidative damage of cell membranes. It has also been recognised Hydroquinone transports rapidly into the vascular system to liver. It has been banned for use by the European Committee (24th Dir 2000/6/EC).
Treatment options:
- Microderm will remove dead cell build up thus brightening skin. it will not in itself help unless pigmentation is extremely superficial, but it will help penetration of some serums that could be useful in inhibiting tyrosinase.
- Peels – if pigmentation is in the epidermis a course of peels such as AHA, BHA, retinoids, TCA, resorcinol, may help remove it however not all peels are suitable for darker skin types or Asian skins
- Skin needling – stimulates wound healing response which promotes collagen and restores keratinocyte function. Treatment for melasma should only be done at .25 depth with no pin point blood response. Retinol, Tranexamic or Gluthathione can be applied after.
- Vampire facial– activates 80% of growth factors.
- IPL tends to be better suited in treating epidermal pigmentation, whereas laser is deeper and can be better suited for darker skins as the deeper wavelength can bypass the surface pigment. Laser is selective and will only target the pigmented skin but it not suitable for melasma. There is an increased chance of hyper pigmentation as heat is a major trigger in the cause of pigmentation.
- Cryotherapy –freezing with liquid nitrogen. Great for solar Lentigines and freckles.
- Red light therapy-red wavelength stimulates the mitochondria. A 2017 studypublished in the International Journal of Women’s Dermatology identified red light therapy as a potential treatment for hyperpigmentation, especially for patients who were using more traditional treatment but wanted to experience an “accelerated pace of improvement”. This study reports that light therapy accelerates the removal of melanin without inhibiting melanin production itself. Ultimately, red light therapy can be used to improve hyperpigmentation by itself or in conjunction with other hyperpigmentation treatments. Red light therapy may also offer a degree of protection from ultraviolet light that could reduce the effects of sunlight on hyperpigmentation. A 2016 study published in the Journal of Photochemistry and Photobiology B showed that exposing skin to certain wavelengths of red light lessened skin damage caused by ultraviolet light. (taken from Mito website)
Melasma
Presents as brown patches on the face. It is particularly common in hormone fluctuations such as in pregnancy, hormone treatments, and the pill or IUD. Low levels of the thyroid hormone can also play a factor. UV worsens condition because it causes inflammation which stimulates the melanocyte to produce more melanin. Studies on antihistamines have been shown to help through their action upon mast cells (proliferent in melasma sufferers) and histamine and chemical mediator release. DAO which is an enzyme naturally found in the body and breaks down histamine. VIT C and zinc can also support DAO. 3000mg Vit C to reduce histamine.
Stress hormone cortisol has also been shown to contribute to melasma due to inflammatory nature. Research found links with alopecia and melasma as they are both stress related. Further links are found with melasma and fibroids (growths in the uterus). When Fibroids were removed melasma faded. Fibroids are connected with too much oestrogen. There is involvement of telangiectasia due to an increase in VEGF, which is a growth factor that increases formation of new blood vessels resulting in vascular proliferation. This is thought to drive increased chemical mediator release and thereby increased melanocyte activity. Basement membrane is weakened. Be wary of too much overstimulation of active ingredients eg (retinol).
An interesting Korean report I will be investigating further was drawing links with dysfunctions in liver, spleen and kidney to melasma. Watch this space for the next update on pigmentation blog.
IMPORTANT NERDY SCIENCE STUFF: Sunscreen, UV and Bluelight and EMS
You may be familiar with the above image but not really understand what it represents. This is known as the Electromagnetic Spectrum. Electromagnetic spectrum is the entire range of radiation that the sun produces and emits, a part of which is received by our planet earth’”. (Ahhh…firstly…..wow, who knew the sun emitted Xrays?!!!)
Ok, so key question is, ‘what does the earth receive?’ Anything on the left hand side of UVC is super bad for us, but thankfully it cannot reach the earth. Anything on other side of visible light is not cell changing. So, this just leaves the region of UVB to Infrared that we need to concern our self with.
So, starting with sunscreen: Sunscreens need to advise a SPF rating. This rating refers only to UVB. Which means it will only protect from the suns BURNING rays. Most of us know there are 2 other UV rays A and C. Where do they fit in. As mentions UVC cannot reach earth so forget about that one. UVA however is quite a different story. It penetrates deeper than UVB so it doesn’t burn on the top of skin in the same way. Because it doesn’t burn, we thought it was safe for a long time. It’s only fairly recently, that science has realised it is responsible for cellular ageing and disease (cancer) of cells.
The EMS diagram demonstrates the range of sunlight that reaches the earth. UV is only 8% of sunlight. Visible light (HEV) is 42% and infrared is nearly 50%. Remember, we currently only have sunscreen regulations that protect us from UVB only.
Bluelight
Blue light is similiar in wavelength to UVA as they overlap slightly on the radiation spectrum. It is the reason we see the sky as blue. We are hearing more lately about blue light because it is also the wavelength in our devices such as computers, TVs and phones. Our retinas can actually activate the melanin process just be seeing bluelight. Hence why blue light glasses are now so heavily marketed. We know it can affect our circadian (sleep) rhythm but some studies are also suggesting that it causes pigmentation and oxidative stress and can generate MORE reactive oxygen species (ROS) than UVA and UVB combined. This can lead to inflammation, impaired healing, compromised melanogenesis, sensitivity, dryness, wrinkles, uneven tone and texture and sagging skin.
Infrared
65 % of IR reaches the dermis. It is the heat we feel from sunlight. Too much heat can be detrimental to the skin as it increases the production of melanin and can worsen pigmentation conditions such as melasma. When the skin is exposed to IR it converts to heat and can raise skin temperature by many degrees, thus triggering inflammatory cells and causing DNA damage. It induces free radical production in DERMIS and generates ROS leading to reduced antioxidant capacity and oxidative stress. It is also shown to upregulate the expression of an enzyme that breaks down collagen.
Conclusion
1 Find a sunscreen that has bluelight and infrared blockers and wear every day, especially in front of the computer. Medik8 have a great one as well as blockers in their day cream. Which co-incidentally we sell!!
2 If you have sun spots and freckles these can be easily treated with laser or cryotherapy, and then to prevent recurrence ‘wear sunscreen’.
3 If you have melasma do not go near laser. Try some needling at recommended shallow depth and ingredients that will block the pigmentation pathway at a number of points. What might work for one person may not work for everyone. We recommend Vit B and C which are great antioxidants as well as blockers, and try Tranexamic Acid to support Vitamin B with the vascular component of melasma.
Feel free to make an appointment to discuss how we can help with your pigmentation issues.
Sources : professional beauty, Adam Sheridan, spa and clinic Chrys Antoniou and Jennifer Hookman, spa and clinic, Andrew Christie, APAN- Terry Everitt a deeper look into pigmentation and melasma. The melanogenesis and mechanisms of skin‐lightening agents – existing and new approaches – Gillbro – 2011 – International Journal of Cosmetic Science – Wiley Online Library Dermatol, Science Direct, Bio med central, pubmed: